Abstract
Background:
Acute myeloid leukaemia (AML) arises from the transformation of hematopoietic stem and progenitor cells. Targeting BCL-2 with the BH3-mimetic venetoclax (VEN) has emerged as a highly efficacious treatment option for elderly patients with AML, in combination with either low-dose ara-C (LDAC) (Wei, ASH 2017) or hypomethylating agents (HMA) (Di Nardo, Lancet Oncol 2018). Long-term survival outcomes, however, remain poor among patients with adverse risk karyotype, who often harbour mutations in the TP53 gene. Identification of more effective treatment options with TP53 independent activity represents an area of high unmet therapeutic need in AML.
Methods:
Panobinostat (histone deacetylase inhibitor; HDACi) was obtained from Novartis, S55746 (BCL-2 inhibitor) was obtained from Servier, and venetoclax (BCL-2 inhibitor) was obtained from Selleck Chemicals. Primary AML samples were obtained from patients providing informed consent. For in vivo experiments, NOD/Rag-/-/Il2rgtm1Wjl Tg(IL3, CSF2, KITLG) (NRG-SG3) mice were used. Dosing for S55746 was 100mg/kg daily Mon-Fri and panobinostat 10mg/kg on Mon/ Wed/ Fri.
Results:
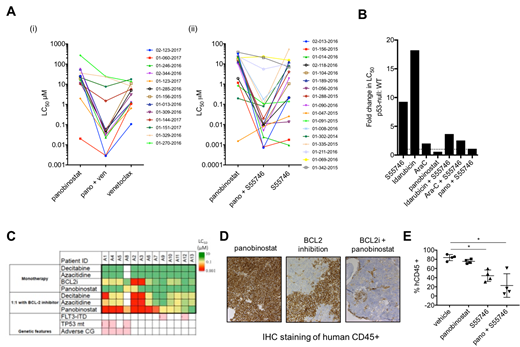
A panel of 22 drugs were screened for enhanced anti-leukaemic activity in combination with BH3-mimetics targeting either BCL-2 or MCL1 against 45 primary AML patient samples. This revealed the histone deacetylase inhibitor (HDACi) panobinostat to have substantially enhanced efficacy: LC50 at 48h was reduced by >2 logs when combined with VEN to target BCL-2 in 13/21 (62%) or S55746 in 19/24 (79%) cases. Targeted exome sequencing revealed adverse-risk AML, including TP53 mutant cases, to be sensitive to this combination. Studies performed in factor dependent myeloid (FDM) cells, derived from gene knockout mice, demonstrated cell death from panobinostat to be Bax/Bak dependent. CRISPR/Cas9 BIM (MV4;11) and TP53 (OCI-AML3) deleted AML cell lines confirmed panobinostat-VEN activity to be independent of these pathways. Comparison of panobinostat in combination with BCL-2 targeting showed the combination to be less affected by p53 deficiency than cytotoxic (idarubicin, ara-C) + BCL2 inhibitor combinations. Patient-derived xenograft (PDX) models confirmed that this combination was tolerable and able to rapidly suppress bone marrow AML in vivo. Exploratory CyTOF and Western blot studies in MV4;11 cells showed that panobinostat +/- BCL-2 targeting markedly suppressed levels of MYC, pSTAT5 and pERK.
Conclusions:
Combined targeting of HDAC and BCL-2 represents a promising, chemotherapy-free, treatment option for patients with AML, including sub-groups with adverse risk genomic characteristics. The combination may have particular relevance for patients with adverse risk AML, including cases defective in functioning TP53.
Teh:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Kraus-Berthier:servier: Employment. Kloos:Servier: Employment; Novartis: Other: Partnership. Schoumacher:Servier: Employment. Gray:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Wei:Celgene: Honoraria, Other: Advisory committee, Research Funding; Novartis: Honoraria, Other: Advisory committee, Research Funding, Speakers Bureau; Amgen: Honoraria, Other: Advisory committee, Research Funding; Pfizer: Honoraria, Other: Advisory committee; Servier: Consultancy, Honoraria, Other: Advisory committee, Research Funding; Abbvie: Honoraria, Other: Advisory board, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal